
Dr. Beaumont, who specializes in brain, skull base and pituitary tumor surgery, shares what drew him to the specialty and why he’s optimistic about the future of brain cancer care.
Meet neurosurgeon-scientist Dr. Thomas Beaumont
Over the past decade, technological advances in minimally invasive surgery, augmented reality and AI have made brain surgery safer and more effective than ever before. Parallel scientific advances—particularly the advent of computational biology—have deepened our understanding of tumor genetics, resulting in a field that is on the cusp of delivering effective brain cancer therapies.
In honor of Brain Tumor Awareness Month, we caught up with Thomas Beaumont, MD, PhD, assistant professor of neurological surgery at UC San Diego Health, to learn how he is using these advanced technologies to provide exceptional care for his patients, discuss his latest brain cancer research and glean his predictions for the future of brain cancer care.
Interviewing Dr. Beaumont
Why did you decide to become a neurosurgeon-scientist?
I’ve always loved science and medicine and people, and was delighted to discover I could combine these three passions as a physician-scientist. I’ve also always followed the moral imperative to use your skills to do as much good as you can in the world. I felt if I could be a great doctor and scientist—who was lucky enough to make a seminal discovery that changes how medicine is practiced—I could maximize my positive impact on the world.
My interest in brain tumors and awake brain surgery began when I was an undergraduate student working in a tumor genetics laboratory and had the opportunity to see awake language mapping surgery. I was immediately hooked and at that moment became dedicated to pursing training in neurological surgery. I obtained a PhD in genetics in a combined MD-PhD training program and after several years of studying epilepsy, returned to brain tumor research.
What are your primary areas of expertise?
My main areas of expertise are treating intrinsic tumors that involve language and motor areas and skull base tumors, particularly those of the anterior skull base and pituitary. I’m skilled in the use of stimulation mapping and awake surgery, advanced imaging with high-resolution diffusion tensor tractography and augmented reality to treat intrinsic tumors. I’m also an expert in the endoscopic endonasal approach (EEA), a minimally invasive technique for treating anterior skull base tumors.
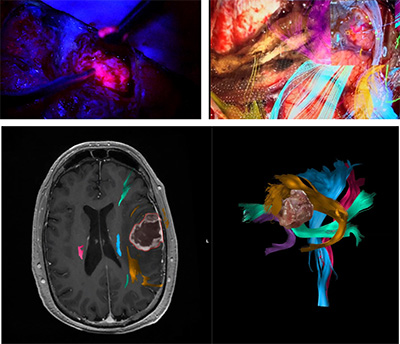
Dr. Thomas Beaumont uses state-of-the-art neuroimaging technologies, including stimulation mapping and augmented reality with high-resolution diffusion tensor tractography, to visualize key structures of the brain and enable safer and more effective surgeries.
What makes the brain tumor program at UC San Diego Health unique?
Our brain tumor program is the most comprehensive in the San Diego region, performing nearly 350 brain tumor surgeries each year. As the only National Cancer Institute-designated Comprehensive Cancer Center in San Diego County, we are a destination center for the most complex brain cancer care.
One of our program’s core strengths is our multidisciplinary approach. For example, our awake surgery team is a closely knit group of neurologists, electrophysiologists, neuropsychologists, and neurosurgeons who are all leaders in their individual fields. We hold a weekly multidisciplinary clinic that gathers treatment perspectives from neuro-oncologists, neurosurgeons, care navigators and social workers to ensure patients receive the best care possible. We also have a multidisciplinary brain tumor board—comprised of neuro-oncologists, radiation oncologists, neuropathologists, and neurosurgeons—that review patient cases on a weekly basis.
UC San Diego Health is also uniquely home to many state-of-the-art surgical technologies. We are home to the only intraoperative MRI in Southern California and one of only four on the West Coast, which allows us to perform both intraoperative scans and minimally invasive procedures such as laser interstitial thermal therapy (LITT) without leaving the OR. We also perform advanced neuroimaging with high-resolution diffusion tensor tractography for augmented reality, together with stimulation mapping, that allows us to visualize and preserve critical structures in the brain during surgery.
When you joined UC San Diego Health in 2019, expanding the skull base tumor program was a key goal for the department. Could you tell us more about this program today?
Our skull base tumor program is a high-volume, multidisciplinary program with dedicated teams at every step of patient care. We perform more than 200 surgeries each year and are the only program in San Diego County offering expanded endoscopic endonasal surgery for anterior skull base meningioma, craniopharyngioma, chordoma and aggressive sinonasal cancers.
The expanded endoscopic endonasal approach offers excellent patient outcomes without making an incision on the head. However, this approach requires specialty training, meticulous surgical technique and a significant investment by the medical center given the wide array of specialized instruments and technology required. I’m grateful that UC San Diego Health has invested in our EEA infrastructure and delighted to see the incredible patient outcomes that this technology enables.
Our multidisciplinary team is comprised of dedicated ENT surgeons, neurosurgeons, pituitary endocrinologists, neuro-ophthalmologists and radiation oncology specialists who are all extremely comfortable treating even the most challenging anterior skull base tumors. This range of expertise was recently recognized by the North American Skull Base Society which named UC San Diego Health a “Multidisciplinary Team of Distinction.” This designation is based on meeting NASBS membership criteria in all necessary specialty disciplines.
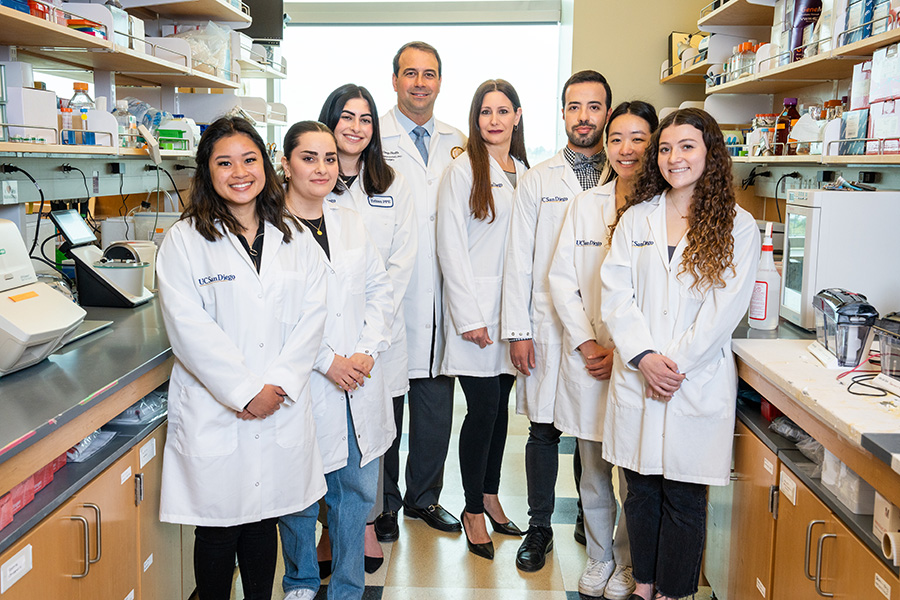
Dr. Thomas Beaumont’s lab, which he co-leads with Dr. Najla Kfoury-Beaumont (center right), is working to develop precision therapeutics for brain cancer by studying chromatin remodeling enzymes, which are believed to drive the development of cancer. Halting this process may prevent early-stage cancers from becoming aggressive, difficult-to-treat tumors.
As a neurosurgeon-scientist, you also run your own lab. Could you tell us more about your current research?
We’re working to develop precision therapeutics for brain cancer by studying chromatin remodeling complexes. These multi-subunit complexes control how tightly DNA is wound, and thus, if genes are able to be turned on, and how much they can be turned up or down—akin to turning the volume up or down on the genome. We believe that chromatin remodelers are key drivers of the development of cancer, so if we can halt this process, we may be able to prevent early-stage cancer from progressing to more aggressive, difficult-to-treat tumors.
In collaboration with investigators at the Salk Institute, we are using single-cell epigenetics techniques to understand how these complexes change their function spatially throughout a given tumor, referred to as clonal heterogeneity. This variation is a significant aspect of why malignant brain tumors are so challenging to treat, so we are hopeful our research will uncover new targets for better treatment options.
I’m also passionate about building resources that accelerate neuroscientists’ quest to understand the brain in health and disease. I am involved in developing AI-based tools to model brain tumors and the associated brain structures to improve the safety of brain tumor surgery and more objectively assess outcomes. I’m honored to serve as deputy director of the UC San Diego Moores Cancer Center Biorepository that banks high-quality tumors, blood and other tissues to support translational cancer research. It is my hope that we can develop a UC-wide cancer consortium to facilitate tissue and data sharing that would greatly accelerate progress toward new therapeutics.
What are your predictions for the future of brain cancer treatment?
The future for brain cancer treatment is bright. We’re approaching an inflection point in the next several years to a decade, where I believe all the scientific knowledge we have gained about brain tumors—and how incredibly complicated they are—will result in new life-saving treatments. Just this week, the first new therapeutic for malignant brain tumors in more than two decades, a targeted therapy called vorasidenib, received FDA fast track designation after it clearly demonstrated improved survival for patients with low-grade glioma.
Additionally, in the next decade we will see the convergence of three areas: tumor epigenomics, advanced imaging and artificial intelligence. In the near future, a patient’s MRI scan won’t look gray and black and 2D; it will be a volumetric rendering of the brain that immediately, using complex AI algorithms, queries databases that will give a neurosurgeon or neuro-oncologist a probabilistic map of the cellular and molecular makeup of the tumor, and the cocktail of targeted drugs that are necessary to treat it. I believe this will all translate to improved patient outcomes and markedly increased survival—hopefully even a cure.

Dr. Beaumont and his family at Del Mar
beach in San Diego
When you aren’t working, what do you like to do for fun?
I try to spend as much time with my family as I can. While neurosurgical oncology requires dedication to one’s patients and perpetual long hours, I have young children whose remarkable growth serves as a constant reminder of the importance of prioritizing family.
Additionally, I like to stay fit and ride bicycles—I have a road bike—and play tennis, despite typically losing to my wife who is a former collegiate player. I also love to sail and be outdoors. I feel incredibly fortunate to live in a city where it’s possible to enjoy these activities year-round.
To learn more about UC San Diego Health’s brain tumor program, visit https://health.ucsd.edu/care/cancer/cancers-we-treat/brain-tumor/
